What is Amoebiasis?
Amoebiasis, an intestinal infection caused by the parasite Entamoeba histolytica, is a significant public health concern in Kenya, particularly in regions with limited access to clean water and proper sanitation. While the parasite itself can be present without causing symptoms, invasive amoebiasis can lead to severe diarrhea, abdominal pain, and even life-threatening complications. Accurate diagnosis is crucial for prompt treatment and preventing further spread.
This article explores the various laboratory techniques employed in diagnosing amoebiasis in Kenya, outlining their advantages, limitations, and suitability within the Kenyan context.
Key takeaways: Diagnosing Amoebiasis in Kenya
- Amoebiasis, a parasitic infection, is a significant public health concern in Kenya.
- Accurate diagnosis is crucial for prompt treatment and preventing spread.
- Stool microscopy is the most common diagnostic tool due to affordability and accessibility, but may lack precision.
- Antigen detection tests offer increased accuracy but can be more expensive and less available in some regions.
- Stool cultures are considered the gold standard but are time-consuming, require specialized expertise, and are costly.
- Molecular techniques provide high accuracy but are currently more expensive.
- The best diagnostic approach depends on factors like cost, availability, and the need for definitive diagnosis.
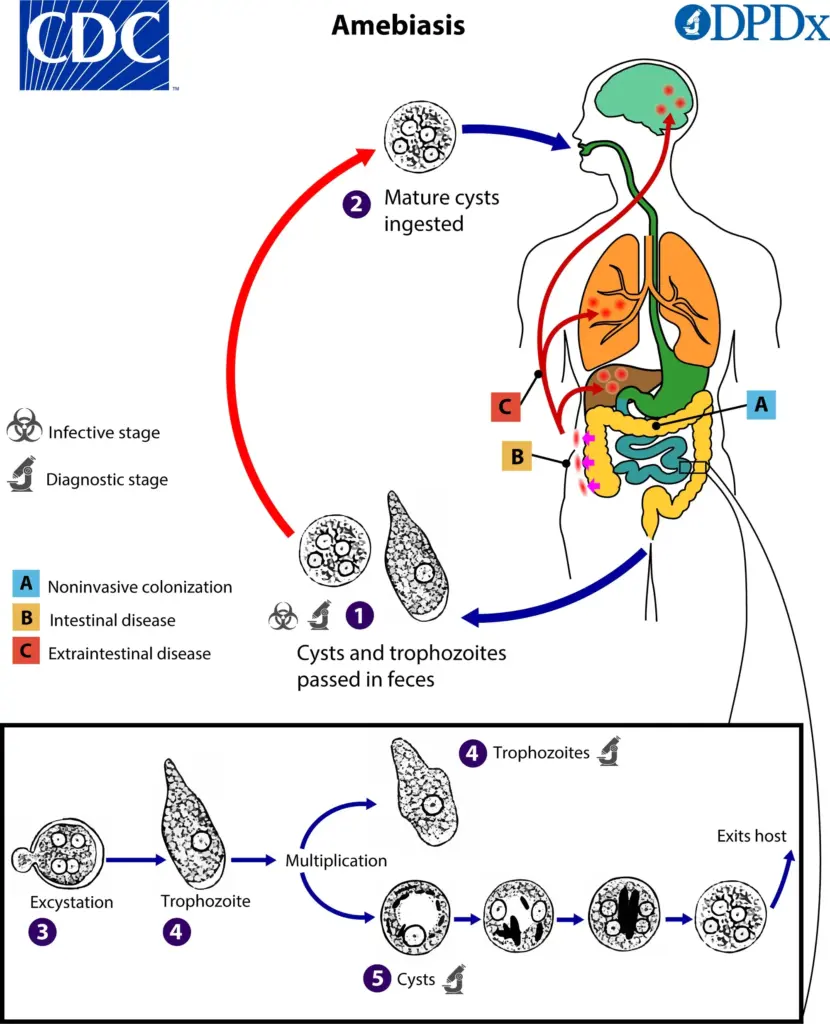
Illustration: CDC
1. Stool Microscopic Examination: The First Line of Defense
Microscopic examination of stool samples remains the most widely used and readily available diagnostic tool for amoebiasis in Kenya. This technique involves analyzing a stool specimen under a microscope to detect the presence of motile trophozoites (active feeding stage) or cysts (dormant stage) of E. histolytica.
Advantages:
- Cost-effective and readily available: Stool microscopy is a relatively inexpensive and simple procedure, making it accessible in most healthcare settings across Kenya.
- Rapid results: Results can be obtained within minutes, allowing for swift initiation of treatment if necessary.
Limitations:
- Sensitivity: Stool microscopy may not detect all cases of amoebiasis, particularly those with low parasite burden.
- Specificity: Microscopy cannot definitively differentiate between pathogenic E. histolytica and non-pathogenic amoeba species like Entamoeba dispar. This can lead to misdiagnosis and unnecessary treatment.
- Technical expertise: Accurate identification of amoeba requires trained personnel with experience in stool microscopy.
Suitability in Kenya: While limitations exist, stool microscopy remains a valuable first-line diagnostic tool due to its affordability and accessibility. However, it’s often recommended to combine it with other methods for a more definitive diagnosis.
2. Antigen Detection Tests: Enhancing Diagnostic Accuracy
Antigen detection tests offer a more specific approach to diagnosing amoebiasis. These tests utilize antibodies that bind to specific antigens (proteins) present on the surface of E. histolytica. A positive test result signifies the presence of the parasite in the stool sample.
Advantages:
- Increased Specificity: Antigen detection tests can accurately differentiate E. histolytica from non-pathogenic amoeba species, leading to fewer misdiagnoses.
- Non-invasive: These tests require only a stool sample, eliminating the need for more invasive procedures.
Limitations:
- Cost: Antigen detection tests can be more expensive than stool microscopy, potentially limiting their widespread use in some Kenyan healthcare facilities.
- Availability: Compared to stool microscopy, antigen detection tests may not be as readily available in all regions of Kenya.
Suitability in Kenya: Antigen detection tests offer a valuable tool for confirming positive stool microscopy results or diagnosing cases where microscopy is inconclusive. However, cost and availability considerations need to be factored in.
3. Stool Culture: The Gold Standard (with Limitations)
Stool culture is considered the gold standard for diagnosing amoebiasis in Kenya. In this technique, a stool sample is placed in a specific medium that allows E. histolytica to grow. After incubation, the culture is examined for the presence of live parasites.
Advantages:
- High Sensitivity: Stool culture can detect even low parasite burdens that might be missed by other methods.
- Differentiation: It can potentially differentiate between E. histolytica and other amoeba species, although additional tests might be needed for confirmation.
Limitations:
- Time-consuming: Stool culture results can take several days to a week, delaying treatment initiation.
- Technical Expertise and Infrastructure: This technique requires specialized expertise and laboratory facilities, which may not be readily available in all Kenyan settings.
- Cost: Culture is generally more expensive than other diagnostic methods.
Suitability in Kenya: While stool culture offers high accuracy, its limitations make it less practical for routine diagnosis in many Kenyan healthcare settings. However, it can be valuable for confirming cases with inconclusive results from other tests or for situations where a definitive diagnosis is critical.
4. Molecular Techniques: A Modern Approach
Molecular techniques, such as Polymerase Chain Reaction (PCR), are gaining traction in diagnosing amoebiasis. PCR amplifies specific DNA sequences unique to E. histolytica, allowing for highly accurate parasite detection.
Advantages:
- High Specificity: PCR can definitively differentiate E. histolytica from other amoeba species.
- Sensitivity: PCR can detect very low parasite burdens
Conclusion
Amoebiasis in Kenya remains a significant public health concern. Selecting the most appropriate diagnostic test depends on several factors, including cost, availability, and the urgency of a definitive diagnosis. Stool microscopy, due to its affordability and accessibility, serves as the initial diagnostic tool in many Kenyan settings. However, for confirmation or in cases with inconclusive microscopy results, antigen detection tests or stool cultures can be valuable. Molecular techniques offer the highest accuracy but are currently limited by cost. As healthcare infrastructure strengthens in Kenya, a wider range of diagnostic options may become more readily available. Regardless of the chosen method, early and accurate diagnosis of amoebiasis is essential for effective treatment, preventing complications, and ultimately, reducing disease burden within the Kenyan population.
